
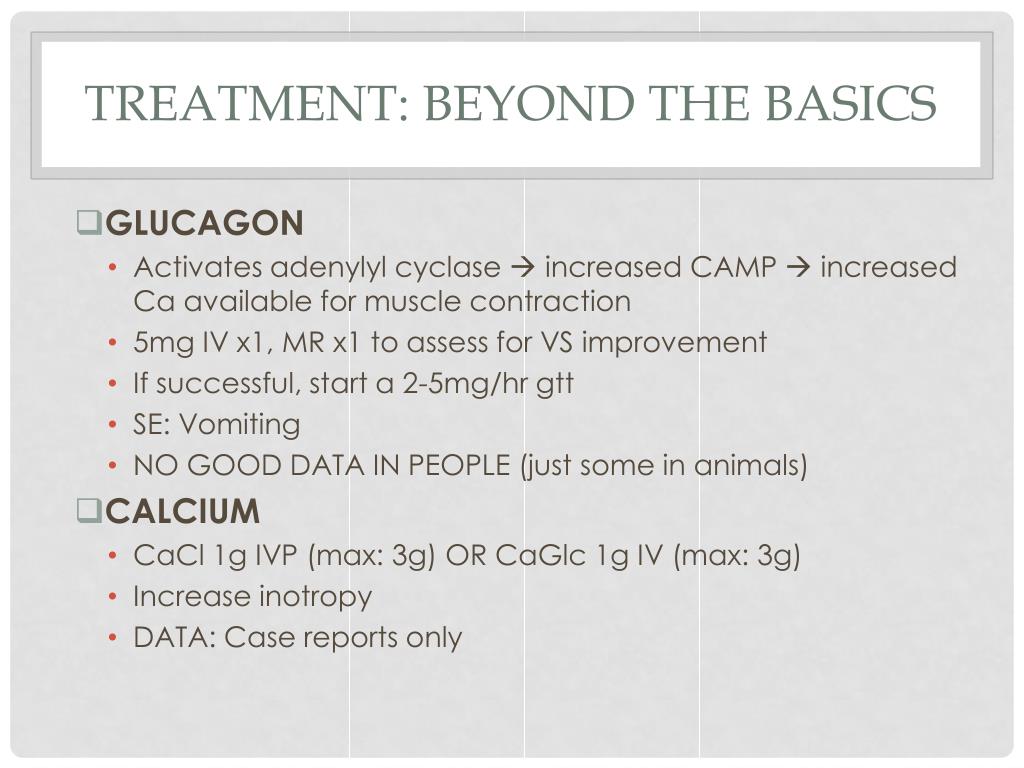
Consider checking acetaminophen and salicylate levels if coingestion is possible. Consider checking TSH, Lyme serology (if no definite history of medication ingestion). Digoxin level, for patients taking digoxin. Chemistries (including Ca, Phos, & Mg). Fingerstick glucose if altered mental status. BBl with sodium channel blockade activity may also cause QRS widening, tall R-waves in aVR, and a Brugada pattern. Any BBl or CCB may cause bradycardia and various heart blocks. History & physical examination (focusing on medication list and access to various substances). Some investigations to consider may include: The differential diagnosis of bradycardia is listed here.Įvaluation will depend on the clinical context. (4) Peripheral vasodilators (betaxolol, bucindolol, carteolol, carvedilol, celiprolol, labetalol, nebivolol) may cause hypotension due partially to peripheral vasodilation. (3) Cardiac potassium channel blockade (acebutolol, sotalol) may prolong the QTc and cause torsade de pointes. Hypotension can be more severe than one would expect, based solely on the degree of bradycardia. (2) Cardiac sodium channel blockade (acebutolol, betaxolol, carvedilol, oxprenolol, pindolol, propranolol) – may cause QRS widening and monomorphic VT. (1) Lipophilic agents (e.g., propranolol) are more likely to enter the brain and cause delirium or seizure. Higher doses: will affect heart as well (vasodilation combined with bradycardia). Lower doses: can cause a primarily vasodilatory shock state (hypotension with reflex tachycardia). However, at high doses they lose selectivity for the vasculature and suppress the myocardium. Dihydropyridine CCBs (e.g., nifedipine, isradipine, amlodipine, felodipine, nimodipine) initially cause vasodilation. Presentation is marked by early development of hypotension and bradycardia. Nondihydropyridine CCBs (verapamil and diltiazem): Cause myocardial suppression more than vasodilation. Neurologic: Delirium, seizure, coma (may result from brain hypoperfusion, or may be due to lipophilic beta-blockers see below). 
💡 In an undefined intoxication with bradycardia and hypotension, the glucose may provide a clue pointing to either CCB or BBl intoxication.CCB poisoning usually causes hyperglycemia, whereas BBl poisoning may cause hypoglycemia.Cardiovascular: Bradycardia, hypotension, and shock are common.Extended-release formulations or sotalol may present later, with deterioration occurring within 24 hours.
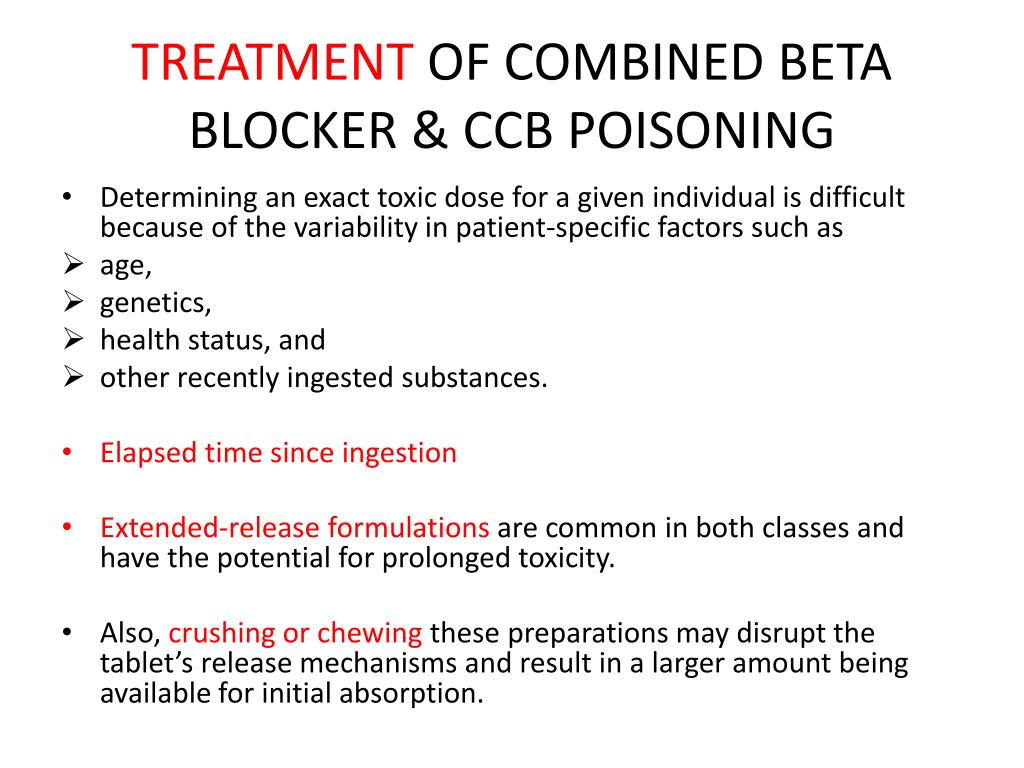
Ingestion of immediate-release formulations should cause clinical deterioration within ~6-8 hours.Onset of symptoms depends on the medication and formulation:.Other issues that may require treatment.





 0 kommentar(er)
0 kommentar(er)
